By Jeb Keiper, CEO of Nimbus Therapeutics, as part of the From The Trenches feature of LifeSciVC. This blog is dedicated to the front-line healthcare workers, essential service workers, scientists, patients, and their families who confront COVID-19 every day, and in reverent remembrance of all of those who have lost their lives to this dread disease.
“You did nothing wrong,” said the Department of Public Health contact tracer who called my spouse late on January 2nd, “you wore a mask and followed all the safety guidelines. We may never know ultimately how you got it.” The sentiment brought no relief – our whole family, myself included, now have Covid.
The major initial feeling, beyond flu-like malaise, is frustration, anger, and helplessness. Doom-surfing upon affliction is a most common response. Before this diagnosis, I tried to stay informed on all things Covid through the amazing journalistic work freely available via many outlets, including blogs, the Timmerman Report, and the amazing community on ‘BioTwitter’. However, I still have come to learn a number of lessons through firsthand experience, which may have improved the trajectory of my disease, and which I would like to share, despite still having active virus.
You are Covid+, Immediately, Do These Things:
- Get Tested. You need your positive PCR test results in-hand, this is the key to unlocking the rest of the kingdom.
- Quarantine. For the love of everything right and holy, I didn’t feel I needed to add this line, but seriously, you can’t leave your home (or room, if others at home aren’t infected) for anything but urgent medical reasons. Stop the spread.
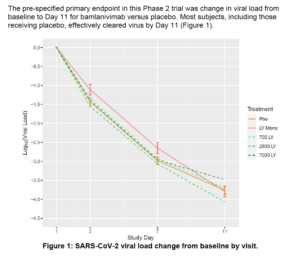
- Sign up to get one of the two Emergency Use Authorization (EUA) antibody regimens (Lilly’s bamlanivimab, or Regeneron’s combo of casirivimab and imdevimab). You can only get these in the first 10 days of symptoms, and they require authorization and an in-clinic, Covid-preped infusion center. These antibodies are one of the few things that will actually work to bring down viral load, and are prescribed to mild/moderate Covid patients who are not-hospitalized, and have a higher risk of progressing to hospitalization. My spouse and I did not qualify as higher risk, while good news, it meant we have to make it through this without intervention. I would note though that the efficacy data itself for the antibodies is not the most stunning (see Figure 1, from the full version of the bamlanivimab EUA):
There are a number of other experimental drug repurposing efforts out there, but many are aimed at hospitalized patients (e.g., remdesivir), or seem cuckoo (the SSRI fluvoxamine to prevent hospitalization).
- Share your news. There is no ‘Scarlet C’. Sharing your condition is not only the right thing to do, but the outpouring of support and monitoring has created essential support buffers during this difficult time. The number of friends and colleagues who have reached out, including a vast number of Covid survivors has been instrumental to our navigating this disease, and their experiences have helped improved ours.
- Consider enrolling in a clinical trial. I’ve been searching to find clinical trials I can qualify for, many are for hospitalized patients, but there are some patient sampling and other trials where your experience can help inform research teams. First interest as a patient has been for something therapeutic, but those seem geared primarily to high-risk individuals, but it is worth trying. Staying proactive, as long as you have the energy, could get you in.
More Lessons From 10 Months of Battle
Some of these surprised me, some made sense the more I learned about the disease from my own body and talking to survivors. Having committed myself long ago to an industry built on the randomized controlled trial, I offer some of the points here with a healthy caveat, that clearly best practice has evolved since Covid landed at the Boston Seaport in March, and will continue to evolve.
- Ventilation. Air circulation is key, we leave windows open on 30-something degree days in Massachusetts with the heat pumping. I can’t imagine what the utility bill will look like, but we have one member of the family who has not tested positive, and ventilating the house, in addition to keeping those of us infected behind closed doors with everyone in N95 masks, is essential.
- Proning. Namely, sleeping on your stomach, not your back. We’ve been following this religiously and I think it really has made a difference to how we feel and the course of the disease staying mild. Avoiding respiratory sequelae is important, though admittedly the benefit for those with more mild / moderate disease has not been studied thoroughly. Here’s a layman’s primer, and a list of active trials studying proning.
- Avoid Exercise. Throughout my life, when feeling a cold approaching, I’d go for a long run. The health benefits, the T cell expansions that occur after vigorous exercise, and the heavy breathing always seemed like a key to good health. For Covid, that could be wrong. Rest, couch potato style, is critical. This Runner’s World article provides a good perspective, and is consistent with the experience a close friend of mine who got Covid back in March from the Biogen conference, a runner, confirms that trying to run while suffering Covid symptoms hampered his longer term recovery.
- Grab Tylenol instead? Pain and aches are a very common symptom of Covid, whether headache, or general myalgia / muscle ache, and so is fever. Earlier in the pandemic, there had been concern that ibuprofen or other NSAIDs could exacerbate Covid, but later refuted in an RCT. So if you have a fever, grab acetaminophen, but if they are pains consider ibuprofen, and if you are well enough to avoid both, great. We used a few doses of acetaminophen in the first few days of symptoms, but have thankfully been able to ween off any OTC meds entirely.
- Covid is never over on day 3. The initial course of Covid, even for adult patients who have mild symptoms and recover, is at a minimum a two week ordeal. (As an aside, I would caveat that many school aged children, my own thankfully included, do seem to ‘recover’ in as soon as 3 days, but just remember they are still contagious!)
As a Covid-ward physician assistant shared with me, “patients often can feel better after 2-3 days, but then take a steep decline. Days 5-7 often see respiratory complications emerge.” Treat this disease with caution, and monitor your condition closely. At home pulse oximeters can be found for about $20, Amazon one, and monitor regularly. If your %SpO2 drops below 95%, call your doctor.
Longer-Term Outlook
My Covid journey is only starting week two as this publishes, so I can’t offer any direct experience, however I can share additional perspectives that have been pouring in. For many Covid patients, life returns mostly to normal after two weeks, but also for seemingly as many, it does not. Weeks to months of lingering symptoms, such as loss of taste and smell, aches and pains, shortness of breath, as well as new symptoms, like gastrointestinal disturbance, neurological symptoms like ‘Covid brain fog’, and others can develop, even for those who never had a hospital stay.
Months ahead, the durability of immune memory to infection comes to mind, “will I be immune?”, perhaps not. A NEJM study indicated an 89% reduction in infection rate over the 6 months after an infection versus naïve patients. Another study showed patients with non-hospitalized Covid clearly have decreases in their IgG titers five months out from infections, which was one of the reasons that the many have called for Covid-recovered patients to get the Covid vaccine in the roll out.
As I write this, over 87 million people have been infected with Covid, over 21 million in the US alone. 1.9 million people dead. Ours is the industry to fight back, and we are. I have never been prouder to work in this industry and am eager to get back to it. While the pandemic rages, patients are still dying from heart disease and cancer, those with autoimmune diseases or other immune-compromising conditions are in a desperate state, and the list goes on. While this has been the most trying time for us, it is also the time when we get back to work and press on with quality science, for the benefit of all.
Many thanks to doctors Alex Harding, Michael Mendelsohn, David Ting, and Nimmi Trapasso, for their clinical advice, care, and help with getting through Covid, and this blog.





